When an ileostomy is performed by a surgical procedure to create an opening which helps attach the ileum to the wall of the abdomen. With an abdominal opening, the surgeon is able to attach your low intestine securely to the abdomen. You will then have a pouch attached on the outside, which all digested material will be collected in.
The purpose of an ileostomy is to bypass the colon or rectum when they no longer work the way they are designed.
Why an Ileostomy is Necessary
There could be many reasons for you to experience intestinal issues that are untreatable. This is why an ileostomy will be necessary. A reason that is most often seen involves inflammation of the bowel, which there are two types: ulcerative colitis and Crohn´s disease.
When ulcerative colitis occurs, there is scarring, inflammation, and sores in and around the rectum and large intestine.
When Crohn´s disease occurs the entire digestive system is involved. It can also easily flare up in the mouth or anywhere in between, which will cause your lining to become inflammed.

Most patients experiencing inflammatory bowel disease will experience pain in the abdomen, bloody stool, deminished nutritional intake, loss of weight.
Getting Ready For Your Ileostomy Surgery
Your life will change after you receive an ileostomy. Nevertheless, your doctor and surgeon will provide you with detailed instructions on how to have an easy time transitioning with the changes.
Ensure your surgeon is aware of all prescription medications that you are currently taking because most of them could have an adverse affect on the way your intestine works. This goes for all medications that are over-the-counter. Be aware that you may need to stop taking certain meds that your surgeon advises you about.
The Ileostomy Process
Since an ileostomy is a surgical procedure that is conducted under anesthesia, it will always take place in hospitals.
Once under anesthesia, a laceration will be made horizontally on the abdomen. The surgeon may also decide to conduct a laparoscopy by using tiny incisions and laparoscopy instruments. Your surgeon will advise you beforehand regarding the best course of action.

A variety of Ileostomies Exist
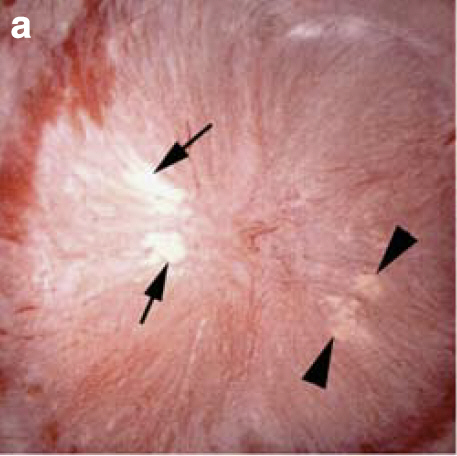
When an ileostomy is conducted, an incision is made which will mark the ileostomy´s placing. A piece of the ileum will be exposed from the incision. This is then folded inside out, with the inside surface exposed. The stoma is the part that will be sticking out for no more than 2 inches.
This ileostomy type is known as a Brooke Ileostomy and does not provide control of when waste is moving.
A continent ileostomy is another ileostomy your surgeon may opt for. This is an internal ileostomy where waste is collected internally. It´s stoma is external and is used as a valve for emptying the pouch.
The continent has several advantages including having an internal pouch along with full control of when the pouch gets emptied. The procedure used is known as a K-pouch. Out of all of the ileostomies available, this one is the most widely used.
Another one is the J-pouch. This one is utilized if the rectumand colon has been taken out. As this procedure is done, an internal pouch is created with the anal canal attached. This will then permit the normal excretion of waste.
Ileostomy Recovery
In most cases, a 3-day stay in the hospital will be required. However, if your ileostomy was conducted as an emergency, then you may need to stay longer for observational purposes.
You will also have a limited amount of intake. A day after surgery you may only get a clear liquid diet. Afterwards, you may progress back to solid foods after the bowels have had time to regulate.
A few days following surgery, an extreme amount of gas may be experienced. It will slow reduce while the healing continues within the intestines.